Scientists could soon remove cancer from the human body with low-power electricity

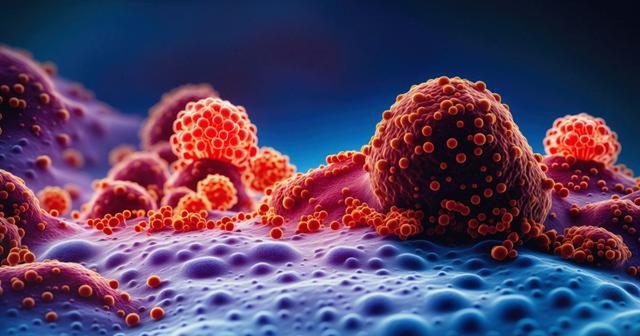
New research from Virginia Tech's Fralin Biomedical Research Institute shows that low-intensity electrical pulse therapy can help prepare the tumor environment for the immune system to function better.
This therapy has not received as much attention as high-intensity focused therapy, which is commonly used to destroy tumors.
Historically, high-frequency irreversible electroporation (H-FIRE) has been established to eradicate tumor masses through targeted electrical disruption of malignant cell membranes.
While effective in direct cytotoxicity, this approach often spares peripheral tumor regions, leaving residual neoplastic activity.
However, H-FIRE induces a significantly different physiological response in its sub-ablative form, delivered at reduced electrical intensity.
Rather than inducing immediate tumor cell death, sub-ablative H-FIRE facilitates rapid remodeling of blood vessels within the tumor microenvironment.
In a controlled study of breast cancer, researchers found that blood vessels increased significantly within 24 hours of treatment. On the third day, they also noticed an increase in lymphatic vessels.
These changes indicate that the tumor adapts its support system, which may improve the body's ability to monitor and move immune cells.
Published in the Annals of Biomedical Engineering, the study documents a shift in focus from the tumor as a target of direct destruction to the tumor as a node of immunological engagement.
By increasing perfusion and lymphatic drainage pathways, the modified environment may enable more efficient recruitment and homing of cytotoxic T cells and other immune effectors.
Lead author Dr. Jennifer Munson, director of the Fralin Biomedical Research Institute's Cancer Research Center, said: "Sub-ablative H-FIRE does not eliminate the tumor completely, but it appears to change the rules of engagement. We are seeing signals that may direct immune cells more effectively to the tumor site through lymphatic pathways."
The study further elucidates a previously underexplored dimension of electroporation-based therapy.
While previous observations had hinted at increased immune activity at partially ablated tumor margins, the functional interaction with the lymphatic system remained poorly characterized.
By examining primary tumor sites and adjacent lymph nodes, the research team has illuminated a pathway by which sub-ablative pulse protocols can potentially enhance the systemic immune response.
These results have important implications for integrative cancer therapy strategies.
There is a promising link between changes in blood vessel structure and cancer treatments such as checkpoint inhibitors and adoptive cell transfer therapies. This offers valuable research opportunities that could lead to new treatments.
Support for the study was provided by multiple groups at the National Institutes of Health, including the National Cancer Institute, the National Center for Advancing Translational Sciences, and the National Institute of Biomedical Imaging and Bioengineering.
Munson notes that future research objectives will focus on mapping the downstream immune responses activated by vascular remodeling and assessing whether these responses can be amplified when sub-ablative H-FIRE is used in conjunction with existing immunomodulatory therapies.
Sub-ablative H-FIRE may not completely cure the cancer, but it can help change the tumor's environment. This change may improve how well the immune system can fight the cancer. This is an important step in the continued development of cancer treatment options.
Happening now...

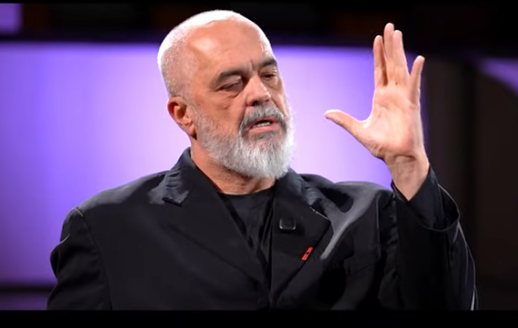
83 mandates are not immunity for Rama's friends
ideas

"Preliminary sentence for Belinda Balluku", response to Baton Haxhiu

Teatri që fsheh prapaskenën

Berisha's red line and the black line of democracy in the DP
top
Alfa recipes
TRENDING 
services
- POLICE129
- STREET POLICE126
- AMBULANCE112
- FIREFIGHTER128